



Frequency of cholelithiasis in patients with Beta-thalassemia intermedia with and without hydroxyurea. Hypogonadotropic hypogonadism in a female patient with thalassemia major. Thalassemia: Complications and Treatment. doi:10.3389/fmolb.2020.00074Ĭenters for Disease Control and Prevention.
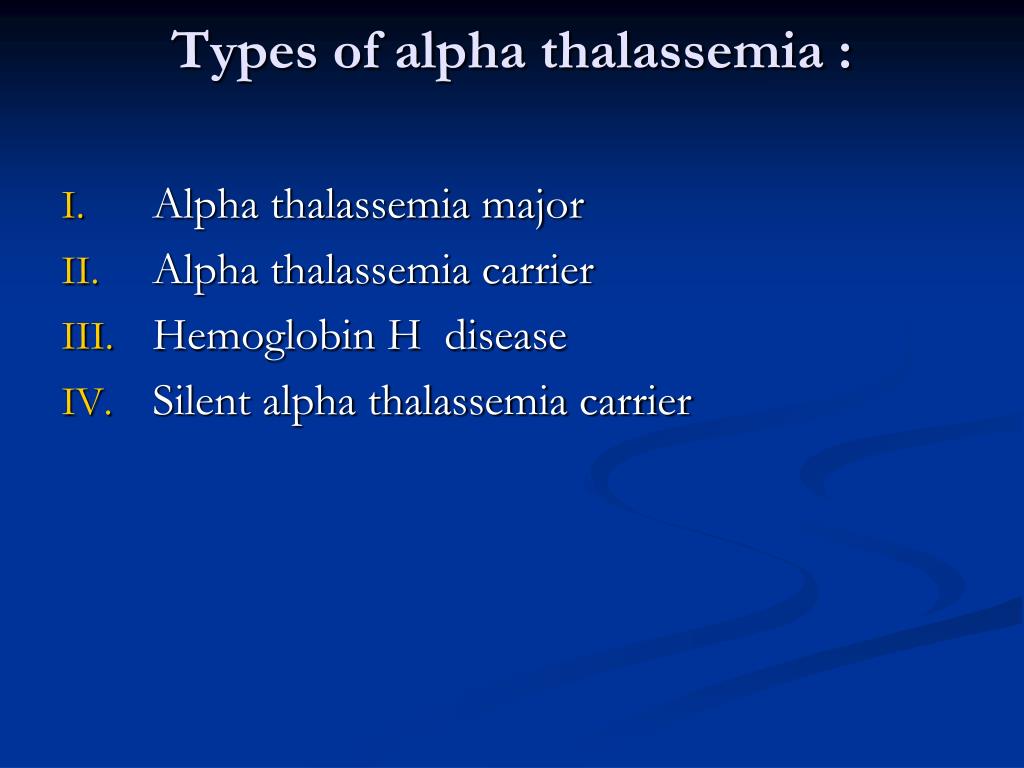
#Alpha thalassemia update
Update in Laboratory Diagnosis of Thalassemia. Munkongdee T, Chen P, Winichagoon P, Fucharoen S, Paiboonsukwong K. Alpha Thalassemia.Ĭenters for Disease Control and Prevention. Chelation: This treatment uses a medication that binds to iron, which is then eliminated from the body via urination or defecation.Tea, particularly black tea, decreases the absorption of iron and may be recommended with meals. Low-iron diet: Because people with thalassemia intermedia are at risk to develop iron overload from increased absorption of iron in the diet, a low-iron diet may be recommended.Hydroxyurea: Hydroxyurea is a daily medication taken by mouth in an effort to increase hemoglobin, thereby reducing the need for RBC transfusions.In these circumstances, splenectomy may be considered. This is often ineffective and may worsen anemia and/or increase transfusion need. Splenectomy: In thalassemia, the spleen may enlarge (splenomegaly) in an effort to improve RBC production.Folic acid: Some physicians may recommend folic acid daily to support RBC production.Transfusion may be needed in times of increased growth and development (puberty), illnesses (particularly those with fever), pregnancy, or in preparation for surgery. Transfusions: People with thalassemia intermedia may require transfusions, but generally not as frequently as people with thalassemia major until adulthood.Routine medical care: Not every person with thalassemia intermedia will require treatment, but it is important to continue close medical care to monitor for complications.It is recommended that people with thalassemia intermedia follow a low-iron diet and drink tea with meals as tea blocks the absorption of iron.
In thalassemia, hepcidin levels are low, allowing more iron to be absorbed than is needed. Increased absorption of iron from food: The body recognizes that the bone marrow is not doing a good job producing hemoglobin and red blood cells. Hepcidin is a protein that blocks the absorption of iron.So over time, these repeated transfusions may result in the development of iron overload, although generally later in life (adulthood) than people with thalassemia major (childhood). Repeated red blood transfusions: Even though children with thalassemia intermedia generally don’t require transfusions every 3 to 4 weeks like children with thalassemia major, they still may require several blood transfusions every year. Each red blood transfusion received is like an intravenous (IV) dose of iron. The body does not have a great way to remove this iron from the body.


 0 kommentar(er)
0 kommentar(er)
